It is concerning when you have sudden hip pain that you many never have experienced before. It may be from something simple like getting up from the sofa or getting out of the car or chair. You may feel like something is catching, can be sharp at times and may even cause you to limp.
It is lasting longer than you like and the hip pain is starting to interfere with your daily activities. You seek medical attention and likely prescribed anti-inflammatories (Aleve, Motrin), heat/ice, stretching maybe even referred for physical therapy and/or deep tissue massage. Fortunately, one or more of these treatments will usually resolve your pain and get you back on track.
What happens if the treatments for your hip pain do not work or in some cases make you worse? MRI’s are often ordered and likely show a “labral tear.” The labrum is the cartilage rim of the hip socket that absorbs shock. The problem is as with most imaging is that the likelihood of seeing a labral tear on MRI is common as we get older, especially if have led an active life.
So, what do you do?
The good news is that most people do not need surgery for hip pain and labral tears.
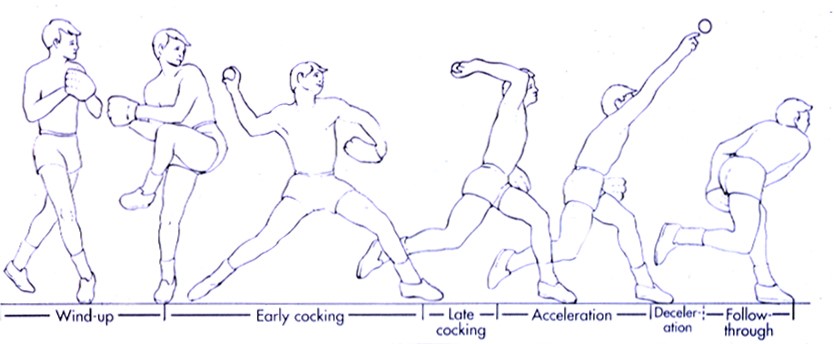
The hip pain is often a combination of “wear and tear” over time with degenerative changes as well as tight/weak hip muscles. The hip needs to be treated as an organ, addressing all the potential issues surrounding the hip.
If the arthritis is minimal, one should consider an ultrasound guided injection under local anesthesia in the office. Prolotherapy, PRP (platelet rich plasma) and Stem Cells (via bone marrow concentrate) have given my patients good relief in most cases. We address the pathology of the whole hip joint-labrum, capsule, cartilage and tendon. It is safe with minimal complications.
To learn more, review the website information and to see if you are a candidate, call the Morgan Kalman Clinic at (302) 529-5500 to request an appointment with Dr. Vic Kalman.